Recently, news broke that a 5-year-old girl in Kerala died of an infection caused by the brain-eating amoeba. The term "brain-eating amoeba" might sound like something out of a horror movie, but it's a real and terrifying organism that exists in our natural environment. Scientifically known as *Naegleria fowleri*. This single-celled amoeba can cause a rare and devastating brain infection called primary amebic meningoencephalitis (PAM). Despite its rarity, the high mortality rate and rapid progression of the disease make it a topic of significant concern. In this blog, we will delve deep into what *Naegleria fowleri* is, how it infects humans, the symptoms and progression of PAM, and what measures can be taken to prevent infection.
What is Naegleria fowleri?
Naegleria fowleri is a thermophilic (heat-loving) amoeba commonly found in warm freshwater environments such as lakes, rivers, hot springs, and even inadequately chlorinated swimming pools. It thrives in temperatures up to 115°F (46°C) and is most commonly found in southern-tier states in the U.S. during the summer months when water temperatures are highest.
Lifecycle and Infectious Stage
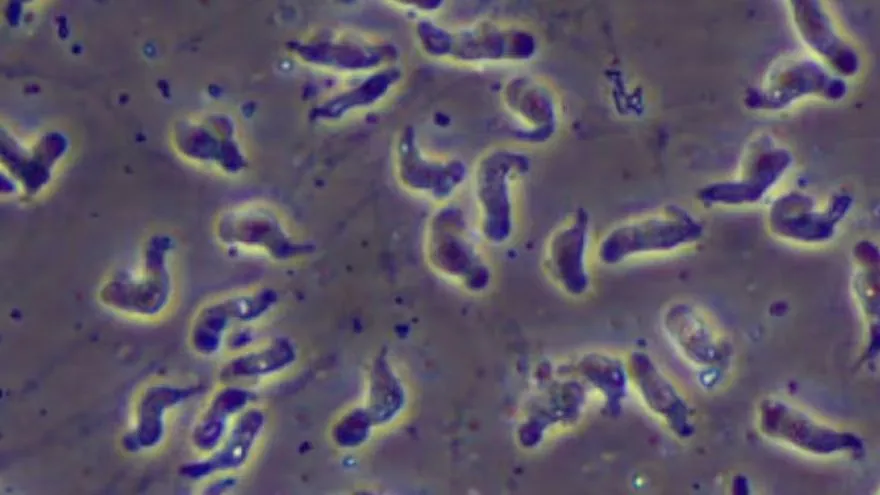
The amoeba exists in three forms during its lifecycle: cyst, trophozoite, and flagellate. The trophozoite stage is the infective form that can cause illness in humans. In this stage, the amoeba is active and feeds on bacteria and organic matter in the environment. When conditions are unfavorable, it can transform into a cyst, a dormant and resilient form that helps it survive. The flagellate form is a temporary stage that the amoeba can transform into when it is in a nutrient-poor environment.
How Infection Occurs
Infection by *Naegleria fowleri* is exceedingly rare but incredibly serious. It occurs when contaminated water enters the body through the nose, typically during activities like swimming, diving, or using unclean water for nasal irrigation. Once the amoeba enters the nasal passages, it travels up the olfactory nerve to the brain, where it begins to destroy brain tissue.
Symptoms and Progression of PAM
The symptoms of primary amebic meningoencephalitis (PAM) or brain eating amoeba usually appear between 1 to 9 days after exposure. The early symptoms are often nonspecific and can be mistaken for other illnesses, which complicates diagnosis. Early symptoms include:
- Severe frontal headache
- Fever
- Nausea and vomiting
As the disease progresses, the symptoms become more severe and can include:
- Stiff neck
- Seizures
- Altered mental status (e.g., confusion, hallucinations)
- Loss of balance
- Sensitivity to light
- Coma
The disease progresses rapidly, often leading to death within about 5 days of the onset of symptoms. The rapid progression underscores the critical need for early detection and treatment.
Diagnosis of PAM
Diagnosing PAM can be challenging due to its rarity and the nonspecific nature of early symptoms. When PAM is suspected, doctors may perform a lumbar puncture (spinal tap) to examine cerebrospinal fluid (CSF). Under a microscope, the presence of *Naegleria fowleri* can sometimes be detected. Advanced diagnostic techniques such as polymerase chain reaction (PCR) and immunohistochemistry can also be used to confirm the presence of the amoeba in the CSF or brain tissue.
Treatment and Prognosis
The prognosis for PAM is generally poor, with a mortality rate over 97%. Treatment typically involves a combination of antifungal and antimicrobial drugs. The main drugs used include:
- Amphotericin B: Administered intravenously and sometimes intrathecally (directly into the CSF) to kill the amoeba.
- Miltefosine: An anti-leishmanial drug that has shown promise in treating *Naegleria fowleri* infections.
- Fluconazole, Rifampin, and Azithromycin: These antibiotics are often used in combination with other treatments to target the amoeba.
Despite aggressive treatment, most patients do not survive, highlighting the critical need for early intervention and new treatment strategies.
Prevention of Infection from
Given the high mortality rate and the limited treatment options, prevention is crucial. Here are some key measures to reduce the risk of infection:
- Avoiding Water-Related Activities in Warm Freshwater: Especially during periods of high water temperature, avoid swimming or diving in warm freshwater lakes, rivers, and hot springs.
- Using Nasal Protection: When engaging in activities like swimming or diving, using nose clips or keeping your head above water can prevent water from entering the nasal passages.
- Proper Pool Maintenance: Ensure that swimming pools, spas, and other recreational water venues are adequately chlorinated and maintained.
- Using Safe Water for Nasal Irrigation: Only use sterile, distilled, or boiled water for nasal rinsing or irrigation.
Cases of PAM are extremely rare, with fewer than 100 cases reported. However, these cases often attract significant attention due to their severity and the devastating impact on affected families. Recent cases highlight the importance of public awareness and the need for rapid medical response when symptoms appear after exposure to warm freshwater.
Research into *Naegleria fowleri* and PAM is ongoing. Scientists are exploring new diagnostic methods, potential treatments, and ways to improve public awareness and prevention strategies. Studies are also being conducted to better understand the biology and behavior of the amoeba, which could lead to more effective interventions in the future.
Conclusion
Naegleria fowleri, the brain-eating amoeba, is a rare but deadly pathogen that poses a significant threat in warm freshwater environments. Understanding its lifecycle, how infection occurs, and the symptoms of PAM is crucial for early diagnosis and treatment. While the prognosis for PAM is generally poor, awareness and preventive measures can significantly reduce the risk of infection. Ongoing research and public health efforts are essential in the fight against this formidable organism. By staying informed and taking appropriate precautions, we can protect ourselves and our loved ones from this terrifying and deadly amoeba.
FAQ: Brain-Eating Amoeba (Naegleria fowleri)
What is Naegleria fowleri?
Naegleria fowleri is a single-celled amoeba commonly referred to as the brain-eating amoeba. It thrives in warm freshwater environments and can cause a rare but severe brain infection called primary amebic meningoencephalitis (PAM).
Where is brain eating amoeba commonly found?
Naegleria fowleri or brain eating amoeba is typically found in warm freshwater bodies such as lakes, rivers, hot springs, and poorly maintained swimming pools. It is most prevalent in southern-tier states in the U.S. during the summer months.
How does Naegleria fowleri infect humans?
Infection occurs when water contaminated with the amoeba enters the body through the nose. This can happen during activities like swimming, diving, or using contaminated water for nasal irrigation. The amoeba then travels up the olfactory nerve to the brain, where it causes infection.
What are the symptoms of primary amebic meningoencephalitis (PAM) or brain eating amoeba?
Symptoms of PAM usually appear between 1 to 9 days after exposure and include:
-
Severe frontal headache
-
Fever
-
Nausea and vomiting
-
Stiff neck
-
Seizures
-
Altered mental status (e.g., confusion, hallucinations)
-
Loss of balance
-
Sensitivity to light
-
Coma
How is PAM diagnosed?
PAM can be diagnosed through a combination of clinical symptoms, patient history, and laboratory testing of cerebrospinal fluid (CSF). Techniques such as microscopy, polymerase chain reaction (PCR), and immunohistochemistry can be used to detect the presence of Naegleria fowleri in the CSF or brain tissue.
What is the treatment for PAM?
Treatment typically involves a combination of antifungal and antimicrobial drugs, including:
-
Amphotericin B (administered intravenously and sometimes directly into the CSF)
-
Miltefosine
-
Fluconazole
-
Rifampin
-
Azithromycin
Despite aggressive treatment, the prognosis for PAM is generally poor, with a high mortality rate.
